Abstract
Background: Compared to de novo AML (dnAML), secondary AML (sAML) is recognized to have worse prognosis regardless of whether it stems from antecedent hematologic disease (AHD) or prior chemoradiation exposure (therapy-related, tAML). This classification is frequently used in determining eligibility for clinical trials or therapies. Additionally, clinicians may consider patients as sAML based on history of antecedent blood count abnormalities in the absence of a pathologically proven AHD. However, the poor prognosis of sAML may reflect the adverse risk genetics that often accompany this label as opposed to the historical features themselves: the European LeukemiaNet (ELN) 2022 risk classification newly incorporates secondary-like genetic features in its adverse risk group, and TP53 mutation underlies the adverse prognosis of many tAML cases. Herein, we evaluated whether AHD, therapy-relatedness, or antecedent blood count abnormalities were independently prognostic after accounting for ELN 2022 risk category and TP53 mutation at time of AML presentation.
Methods: Clinical, histopathologic, cytogenetic, and molecular genetic data were collected on 735 adults with newly diagnosed AML from Johns Hopkins Hospital (JHH; Baltimore, MD) and Massachusetts General Hospital (MGH; Boston, MA). Per WHO criteria, post-AHD sAML cases were identified by prior pathologic diagnosis of AHD (e.g., myelodysplastic syndrome or myeloproliferative neoplasm). tAML cases were identified by history of prior chemoradiation exposure. dnAML cases were evaluated for previous abnormal blood counts at least 28 days and up to 2 years prior to AML diagnosis. AML therapies were categorized as either with curative intent (intense therapies, e.g., 7+3) or not (less intense therapies, e.g., hypomethylating agent/venetoclax therapy or supportive care). Wilcoxon rank-sum and Fisher's exact tests were used to compare groups. Uni- and multivariable Cox models evaluated associations between overall survival (OS) and covariates: age, performance status (PS; ECOG 0-1 as good vs 2-4 as poor), therapy type, ELN 2022 risk group, TP53 mutation, prior abnormal counts, and hematopoietic stem cell transplant status (time-dependent).
Results: Of the 735 patients in the cohort (388 from JHH, 347 from MGH), 410 (56%) had dnAML, 202 (27%) had sAML from AHD, and 123 (17%) had tAML. Of the dnAML patients, 86 previously had normal and 154 had abnormal prior blood counts documented; antecedent blood counts were not available in the remaining patients. AHD and tAML patients were older than dnAML patients (median age 68 and 67 versus 62 years respectively, P<0.001) and more often ELN adverse compared to dnAML (83% and 69% versus 44% respectively, P <0.001). Fewer AHD and tAML patients received curative intent treatment versus dnAML (36% and 43% versus 71% respectively, P<0.001).
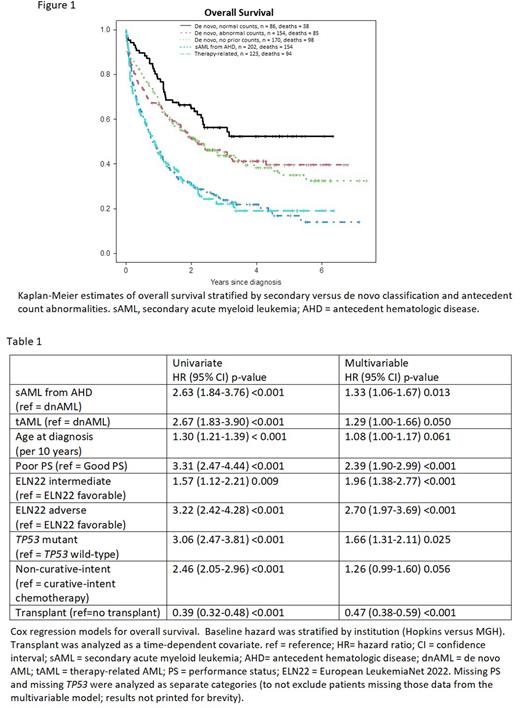
On univariate analysis, dnAML patients had longer OS than AHD and tAML patients; OS of dnAML with abnormal prior counts fell between dnAML with normal prior counts, AHD, and tAML patients (Figure 1). On multivariable analysis controlling for age, PS, ELN risk, TP53, therapy class, and transplant, dnAML with abnormal prior counts lost prognostic significance (hazard ratio [HR] = 1.17 [reference = dnAML with normal prior counts]; 95% confidence interval [CI] 0.79-1.73, P=0.44). In a subsequent multivariable analysis, AHD and tAML were associated with a poorer prognosis compared to dnAML (regardless of prior counts) after controlling for the other model covariates including ELN risk, although the HRs were attenuated from the univariate model (Table 1; univariate vs multivariable: AHD HR=2.63, 95% CI 1.84-3.76 vs 1.33, 95% CI 1.06-1.67; tAML HR= 2.67, 95% CI 1.83-3.90 vs 1.29, 95% CI 1.00-1.66).
Conclusions: In this multicenter cohort, antecedent blood counts did not provide independent prognostic information for de novo AML patients after accounting for ELN 2022 genetic risk and TP53 mutation status. Nonetheless, AHD/tAML maintained prognostic association with shorter OS in the multivariable model, though with reduced effect size by hazard ratio. These findings suggest there remains a role for using secondary vs de novo ontogeny to clinically risk stratify patients, but also emphasizes the greater role genetics (i.e., ELN) should have in risk assessment and clinical trial eligibility in newly diagnosed AML.
Disclosures
Othus:Daiichi Sankyo: Consultancy; Merck: Consultancy; Glycomimetics: Consultancy; Celgene: Consultancy; Biosight: Consultancy. Brunner:Taiho: Consultancy; Takeda: Consultancy, Research Funding; Acceleron: Honoraria; Novartis: Consultancy, Research Funding; Keros Therapeutics: Consultancy; Janssen: Research Funding; GSK: Research Funding; Celgene/BMS: Consultancy, Research Funding; AstraZeneca: Research Funding; Agios: Honoraria; Aprea: Research Funding. Percival:Pfizer: Research Funding; Trillium: Research Funding; Oscotec: Research Funding; Cardiff Oncology: Research Funding; Glycomimetics: Research Funding; Biosight: Research Funding; Celgene/BMS: Research Funding; Abbvie: Research Funding; Ascentage: Research Funding; Telios: Research Funding. Hourigan:The Foundation of the NIH AML MRD Biomarkers Consortium: Research Funding; Sellas: Research Funding; Archer Diagnostics: Other; MissionBio: Other; Qiagen: Other; TwinStrand Biosciences: Other. DeZern:Gilead: Consultancy, Honoraria; GERON: Other: DSMB; Novartis: Consultancy, Honoraria; CTI BioPharma: Consultancy, Honoraria; Bristol Myers Squibb: Consultancy, Honoraria; Syntrix Pharmaceuticals: Research Funding. Estey:Bayer Pharmaceuticals: Research Funding.
Author notes
*Asterisk with author names denotes non-ASH members.